Welcome
Start exploring here! We hope this will be a useful resource to help you find the information you need about cerebral palsy and other childhood-onset disabilities. We want to help you to find answers to your questions – so please let us know what else you would like us to cover. Here we are presenting videos, summaries, research information and other resources.
Read on for more
Ways we can help
1
Family-friendly Books
Discover our collection of family-friendly books featuring accessible, research-based insights. These titles include the perspectives of families and individuals with lived experience, offering valuable guidance while supporting parents on their journey.
2
Free Chapters
We have selected a range of chapters from our books, offering helpful insights and practical tips. Our chapters summaries highlight key points. View the full chapter to explore each topic in more depth.
3
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
4
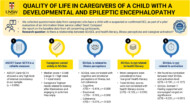
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to more people. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
5
Helpful Videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Gillette Children’s Healthcare Series
The goal of the Gillette Children’s Healthcare Series is to empower families through a greater understanding of their condition and therefore help optimize outcomes for children, adolescents and adults living with these childhood-acquired and largely lifelong conditions.

Free chapter downloads
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
What are the main treatment options for scoliosis?
Treatment options for scoliosis can range from nonsurgical methods, such as observation with repeat X-rays, to surgical methods, such as spinal fusion.
What are the main treatment options for scoliosis?
This answer is adapted from the Gillette Children’s Healthcare Series book on Scoliosis. For more information see Scoliosis – Congenital Neuromuscular, Syndromic, and Other Nonidiopathic Types.
Treatment options for scoliosis can range from nonsurgical methods, such as observation with repeat X-rays, to surgical methods, such as spinal fusion. Treatment options include the following:
- Observation: Regular spine X-rays and clinical exams with a spine specialist to monitor scoliosis curve for possible progression.
- Bracing: A spinal brace that applies corrective forces to the spine to slow or stop scoliosis curve progression.
- Casting: A full-torso cast (hardened plaster or fiberglass that must be cut off to remove) that applies corrective forces to the spine to improve the scoliosis curve (decrease the Cobb angle) or slow or stop scoliosis curve progression.
- Surgery: Surgery performed to prevent future progression and improve the scoliosis curve (decrease the Cobb angle). There are many types of scoliosis surgery. The most common type is spinal fusion, defined as fusing (joining together) two or more vertebrae in the spine; screws and metal rods are typically used to hold the spine in the straightened position and facilitate fusion between bones.
As the child grows, the risk of scoliosis progression may increase or decrease, resulting in treatment plans changing. It is common for an individual to undergo multiple treatment types over the course of their childhood and adolescence. For example, an individual may be observed for a period of time, then prescribed bracing treatment if their curve progresses.
The appropriate treatment chosen and the related goals depend primarily on individual patient goals and specific treatment indications. Indications include, but are not limited to, size of the curve, risk of curve progression, and skeletal maturity of the child.
Treatment indications and goals may vary at other hospitals and treatment centers. Surgical guidelines are general and depend on the surgery type and clinical practice continually evolves.
It is important to note that for most individuals, scoliosis cannot be “cured” (i.e., to achieve a Cobb angle less than 10 degrees). For some children with infantile idiopathic scoliosis, their curve may spontaneously resolve, or casting treatment can reduce the curve to less than 10 degrees, but that is the exception. The more common outcome and realistic goal is to have a small enough residual curve after treatment that will not adversely affect quality of life.
Purchase ‘Scoliosis: Congenital, Neuromuscular, Syndromic and other Nonidiopathic Types’.
Preview full content of the book via Flipbook.
How will scoliosis affect my child’s day-to-day life?
Research shows that individuals treated for scoliosis have physical activity levels comparable to the general population, and most report good mental and social health.
How will scoliosis affect my child’s day-to-day life?
This answer is adapted from the Gillette Children’s Healthcare Series book on Idiopathic Scoliosis.
Research shows that individuals treated for scoliosis have physical activity levels comparable to the general population, and most report good mental and social health.
Potential challenges include:
- Physical discomfort and limitations: Bracing, a common treatment, may cause heat, pressure, and physical discomfort while the brace is being worn. The brace is removed for sports and physical activity. Full-time brace wear can negatively affect quality of life, including emotional stress and social isolation, especially in adolescents.
- Psychosocial impact: Adolescents may feel self-conscious about their appearance, experience embarrassment, or avoid social interactions due to concerns about being different from peers.
- Activity restrictions: Post-surgery recovery involves temporary limitations, such as avoiding twisting, bending, lifting over 10 lb (4.5 kg), or participating in contact sports for several weeks to months. However, these are temporary and part of the healing process. Once healing has happened, most activities can be resumed without restriction or limitation.
While scoliosis may require temporary adjustments—such as wearing a brace or following temporary post-surgical restrictions—the long-term outlook is very positive. With proper treatment, most children can expect to live full, active lives with minimal impact on their daily routines and overall well-being.
Will scoliosis get worse over time?
Scoliosis does not always worsen, but it can progress over time—especially in people whose curves are larger, who are still growing, or who have other risk factors. However, some curves do show a tendency for rapid change, so monitoring is essential to detect any worsening promptly just as each person is unique, so too is the behavior of each scoliosis curve, and the only way for the spine specialist to understand that behavior is through observation. For curves smaller than 20° the risk of rapid progression is lower, so many patients are managed by observation with regular X‑rays and clinical exams to catch any change early.
Will scoliosis get worse over time?
This answer is adapted from the Gillette Children’s Healthcare Series book on Scoliosis. For more information see Scoliosis – Congenital Neuromuscular, Syndromic, and Other Nonidiopathic Types.
Scoliosis does not always worsen, but it can progress over time—especially in people whose curves are larger, who are still growing, or who have other risk factors. However, some curves do show a tendency for rapid change, so monitoring is essential to detect any worsening promptly just as each person is unique, so too is the behavior of each scoliosis curve, and the only way for the spine specialist to understand that behavior is through observation. For curves smaller than 20° the risk of rapid progression is lower, so many patients are managed by observation with regular X‑rays and clinical exams to catch any change early.
Research studies that follow individuals who have not had any intervention are called “natural history studies.” Natural history studies suggest that scoliosis treatment is necessary, and that the timing of treatment is important for best outcomes. Early scoliosis treatment is important to:
- Prevent or delay the need for surgical intervention
- Optimize growth and development of chest and lungs, especially for
individuals with EOS - Minimize surgical risks as individuals with smaller curves are less likely to experience surgical complications than are individuals with larger curves
Not all treatment options are appropriate for every individual. Recommendations for scoliosis treatment are made by identifying the size and location of the curve, age, and risk of the curve progression.
Purchase ‘Scoliosis: Congenital, Neuromuscular, Syndromic and other Nonidiopathic Types’.
Preview full content of the book via Flipbook.
Did anything cause the scoliosis or make it worse – heavy backpack, the mattress they sleep on, their activities?
No —there is no evidence that heavy backpacks, sleeping on a specific mattress, physical activities, or poor posture cause or worsen idiopathic scoliosis.
Did anything cause the scoliosis or make it worse – heavy backpack, the mattress they sleep on, their activities?
This answer is adapted from the Gillette Children’s Healthcare Series book on Idiopathic Scoliosis.
No —there is no evidence that heavy backpacks, sleeping on a specific mattress, physical activities, or poor posture cause or worsen idiopathic scoliosis.
Parents and children often wonder if certain actions caused the condition, but the answer is a clear “no.” Idiopathic scoliosis is a condition of unknown cause (“idiopathic” literally means “of unknown cause”), and while some family predispositions (having parents or siblings with idiopathic scoliosis) may increase risk, the listed factors are not associated with its development or progression.
Submit a question
Let us know what other questions you have. Are there specific topics you would you like us to cover?
Contact us now using the form.
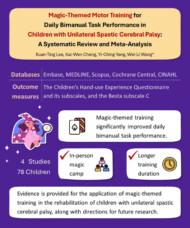
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to individuals with disabilities, parents, caregivers, and others. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
Helpful videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Contact us
Please feel free to contact us if you have any feedback or suggestions: