Welcome
Start exploring here! We hope this will be a useful resource to help you find the information you need about cerebral palsy and other childhood-onset disabilities. We want to help you to find answers to your questions – so please let us know what else you would like us to cover. Here we are presenting videos, summaries, research information and other resources.
Read on for more
Ways we can help
1
Family-friendly Books
Discover our collection of family-friendly books featuring accessible, research-based insights. These titles include the perspectives of families and individuals with lived experience, offering valuable guidance while supporting parents on their journey.
2
Free Chapters
We have selected a range of chapters from our books, offering helpful insights and practical tips. Our chapters summaries highlight key points. View the full chapter to explore each topic in more depth.
3
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
4
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to more people. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
5
Helpful Videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Gillette Children’s Healthcare Series
The goal of the Gillette Children’s Healthcare Series is to empower families through a greater understanding of their condition and therefore help optimize outcomes for children, adolescents and adults living with these childhood-acquired and largely lifelong conditions.

Free chapter downloads
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
How can parents support a child with vision impairment to become more independent and successful?
Parents can encourage their child with vision impairment by treating them like any other child, fostering independence, and promoting the use of assistive technology. Providing emotional support, learning braille or assistive tools together, and ensuring access to resources like mobility training and specialized equipment also enhance independence and self-confidence.
For more information, please read the extract from chapter 21 ‘Personal Experiences from a Young Person’ from ‘Children with Vision Impairment’. Full chapter available to download.
How can parents support a child with vision impairment to become more independent and successful?
Extract from Dale et al., ‘Children with Vision Impairment’, Chapter 21 ‘Personal Experiences from a Young Person’, p. 260
What is important to me as a young person with a vision impairment:
- Being encouraged to strive for success and to have aspirations; having a disability is not an obstacle for success.
- Recognising that every child or young person with vision impairment is different, just like their peers. What works for one person may not work for another.
- Being listened to and understood.
- Remembering that vision impairment is a spectrum and it is important for others to understand what a young person can or cannot see.
- Focussing on the positives of having a vision impairment such as being part of the vision impairment community and proactively acting on these positives.
DMCN articles
For further information, read the below papers on vision impairment in DMCN:
- Interventions for children with cerebral visual impairment: A scoping review
- Autonomy in children and adolescents with visual impairment: Validation of the Visual Impairment Developmental Autonomy scale
- Early visual training and environmental adaptation for infants with visual impairment and its plain language summary
What are some key strategies for parents to manage feeding difficulties in their child with neurodisability, and how can a multidisciplinary team (MDT) support this?
Parents can manage feeding difficulties in children with neurodisability by creating a calm mealtime environment, ensuring proper positioning, using adaptive feeding techniques and equipment, and modifying food textures. A multidisciplinary team (MDT) can provide comprehensive support, including nutritional assessments, caregiver training, and tailored feeding strategies. For more information, please read the extract from chapter 9 of ‘Nutrition and Neurodisability’. Full chapter available to download.
What are some key strategies for parents to manage feeding difficulties in their child with neurodisability, and how can a multidisciplinary team (MDT) support this?
Extract from Sullivan, Andersen and Andrew, ‘Nutrition and Neurodisability’, Chapter 9 (free download), pp. 153-154
Postural Management and Positioning When Eating
Optimal positioning to improve head and trunk stability during mealtimes provides a critical foundation for both safety and efficiency, and is a priority for all children with feeding difficulties (Benfer et al. 2013). Optimal mealtime positioning influences tone and overall patterns of movement, improves coordination of oral motor movements, enhances respiration and airway protection, provides a mechanical advantage for bolus dynamics, positively influences reflux and gut motility, and improves self-feeding (Hulme et al. 1983). Modification of a child’s sitting position from one of generalised extension to greater flexion (particularly at the hips and knees) can facilitate jaw stability and head flexion (Stratten 1981). A stable and aligned head position, achieved both through overall body positioning and specific head support (including head rests or occipital rolls), may improve position, mobility and coordination of the lips, tongue and oral anatomy (Lanert & Ekberg 1995).
Ideal mealtime positioning involves the child seated upright, with 90-degree hip flexion, feet supported, head in midline and aligned on the anterior–posterior plane, and chin slightly tucked. However, no single optimal position exists for all children. Recommendations for mealtime position should be made in collaboration with the child’s physical or occupational therapist, incorporating individualised findings from video fluoroscopy when appropriate and available (Lanert & Ekberg 1995; Gisel et al. 2003). Options for improving mealtime positioning may include specialised seating (infant feeder seats, wheelchairs or supportive chairs); the adaptation of regular seating using pillows, rolled towels, foam and support straps; or postural support by the care-giver’s body. A tray may provide additional postural support and allow stabilisation of the upper limb and shoulder girdle, to achieve a functional sitting position (Stavness 2006). Whilst an upright position is generally advocated, up to 30 degrees of recline, for children who are unstable in an upright position, reduces lip pursing, gag and tongue thrust (Lanert & Ekberg 1995). The upright position may be more beneficial than recline for children with poor pharyngeal clearance or those requiring a slower bolus flow rate (Morton et al. 1993). Flexed head position and chin tuck improves protection of the airway, decreases risk of laryngeal penetration and aspiration and is particularly helpful for children with a delayed swallow initiation (Lanert & Ekberg 1995). Preliminary evidence suggests that reductions in aspiration from improved position, combined with texture modification of food and fluids, translate into longer-term improvements in respiratory function for children with severe feeding difficulties (Gisel et al. 2003).
For an overview of feeding, nutrition and growth in children with complex CP please read chapter 7 of ‘Children and Youth with Complex Cerebral Palsy: Care and Management’, edited by Laurie Glader and Richard Stevenson. Free chapter download.
DMCN articles
For further information, read the below papers on feeding difficulties in DMCN:
- Prevalence of drooling, swallowing, and feeding problems in cerebral palsy across the lifespan: a systematic review and meta-analyses
- Eating and drinking abilities and respiratory and oral health in children and young adults with cerebral palsy and its plain language summary
- Eating and drinking ability and nutritional status in adults with cerebral palsy and its plain language summary
How are children with Down syndrome supported at school?
Children with Down syndrome in mainstream schools should receive support from the whole school, not just teaching assistants. All staff should be trained in their learning needs. Inclusion in the classroom is key, with differentiated curricula, speech and language support, and activities to develop social, literacy, and motor skills, guided by specialists. For more information, please read the extract from chapter 5 of ‘Down Syndrome’. Full chapter available to download.
How are children with Down syndrome supported at school?
Extract from Newton, Puri and Marder, ‘Down Syndrome’, Chapter 5, pp. 41-42.
Some school issues: primary school
Children with Down syndrome in mainstream schools are likely to be supported by one or more teaching assistants (TA). However, support is not the sole responsibility of the TA, but should be a whole school matter. Ideally, all staff in the school should receive training in the learning and communication needs of children with Down syndrome. The child should take part in the life of the school along with his or her classmates. As social skills are a strength, children should be part of the normal class group, not be constantly taken out of the classroom. The curriculum will need to be differentiated according to the needs of the child.
To meet children’s educational needs at primary school, schools need to have a positive attitude towards inclusion and whole school systems to support this outcome, with training for staff about the needs of children with Down syndrome and the use of evidence-based interventions. It will help schools and other practitioners to be aware of the evidence for the benefits of inclusion for children with Down syndrome who do not have additional or complex needs, following a model of full inclusion with a high level of individual support (Buckley et al. 2002; Fox et al. 2004; Turner et al. 2008). The support is likely to include the following:
- Developing self-help skills and personal care, including taking to the toilet,
- Developing play skills—using modelling and imitation strengths,
- Facilitating interaction with peers,
- Delivering differentiated activities under the guidance of the class teacher, particularly for supporting spoken information and listening activities with visual information—signs, gesture, pictures, written words, modelling and repetition,
- Providing daily speech and language activities, guided by the child’s speech and language therapist,
- Providing short periods of additional, focused literacy and language activities, including a daily ‘conversation diary’, whole word reading and phonic programme,
- Providing focused numeracy activities, including use of visual supports,
- Providing practice for developing fine motor skills, guided by an occupational therapist,
- Modelling of drawing and handwriting activities for children to copy,
- Guidance to ensure that children follow routines at school (including using a visual timetable) and maintain positive behaviour.
Successful education will require a flexible approach with school and parents working in partnership.
My child has cerebral palsy and has issues with their sleep, which is causing me to have poor sleep. How typical is this? How can I improve the situation?
Research has shown that sleep problems are common in children with cerebral palsy.
There are a number of things that can be done to improve sleep in children with CP: (1) establishing a regular bedtime routine and sticking to it as much as possible; (2) making sure that the child’s bedroom is dark, quiet, and cool; (3) avoiding caffeine and sugary drinks before bed; and (4) getting regular exercise, but avoiding exercise too close to bedtime.
My child has cerebral palsy and has issues with their sleep, which is causing me to have poor sleep. How typical is this? How can I improve the situation?
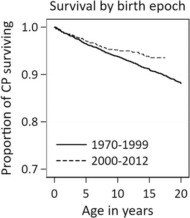
Sleep problems in children with cerebral palsy and their parents
Full paper: https://onlinelibrary.wiley.com/doi/10.1111/dmcn.14920
Plain language summary: https://onlinelibrary.wiley.com/doi/10.1111/dmcn.15810
The study found that sleep problems are common in children with cerebral palsy (CP) aged 0 to 11 years. The most common problems reported by parents were: daytime fatigue, difficulty falling asleep, and early-morning waking. Children with CP were also more likely to have sleep problems than typically developing children, and children with CP who cannot walk were more severely affected by sleep problems than children with CP who can walk.
Parents of children with CP were more likely to report feeling sleep-deprived than parents of typically developing children: one-third of parents of children with CP compared to a quarter of parents of typically developing children.
There are many reasons why sleep problems are so common in these children: (1) they may have physical discomfort/pain or stiffness that makes it difficult to fall asleep and stay asleep; (2) many have gastrointestinal problems such as constipation or reflux; (3) some of the medications they take can cause sleep problems as a side effect; and (4) some children with CP have cognitive impairments that make it difficult to understand and follow bedtime routines.
There are a number of things that can be done to improve sleep in children with CP: (1) establishing a regular bedtime routine and sticking to it as much as possible; (2) making sure that the child’s bedroom is dark, quiet, and cool; (3) avoiding caffeine and sugary drinks before bed; and (4) getting regular exercise, but avoiding exercise too close to bedtime.
If you are a parent of a child with CP and are concerned about their sleep, talk to their doctor. They can help you to identify and address any underlying medical conditions or medication side effects that may be affecting their sleep. They can also provide you with tips on how to establish a regular bedtime routine and create a relaxing bedtime environment.

Practical parenting advice
See the posters of ‘Helping Babies to sleep’ , ‘Help your Child to Sleep’ and ‘How to help teenagers get quality sleep’ for practical advice.
Useful resources:
- Practical parenting advice: https://raisingchildren.net.au/newborns/sleep
- Lullaby Trust which supports research into safe sleeping: https://www.lullabytrust.org.uk/the-lullaby-trust-celebrates-25th-anniversary-of-back-to-sleep-campaign/
Submit a question
Let us know what other questions you have. Are there specific topics you would you like us to cover?
Contact us now using the form.
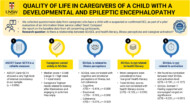
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to individuals with disabilities, parents, caregivers, and others. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
Helpful videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Contact us
Please feel free to contact us if you have any feedback or suggestions: