Welcome
Start exploring here! We hope this will be a useful resource to help you find the information you need about cerebral palsy and other childhood-onset disabilities. We want to help you to find answers to your questions – so please let us know what else you would like us to cover. Here we are presenting videos, summaries, research information and other resources.
Read on for more
Ways we can help
1
Family-friendly Books
Discover our collection of family-friendly books featuring accessible, research-based insights. These titles include the perspectives of families and individuals with lived experience, offering valuable guidance while supporting parents on their journey.
2
Free Chapters
We have selected a range of chapters from our books, offering helpful insights and practical tips. Our chapters summaries highlight key points. View the full chapter to explore each topic in more depth.
3
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
4
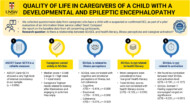
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to more people. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
5
Helpful Videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Gillette Children’s Healthcare Series
The goal of the Gillette Children’s Healthcare Series is to empower families through a greater understanding of their condition and therefore help optimize outcomes for children, adolescents and adults living with these childhood-acquired and largely lifelong conditions.

Free chapter downloads
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
What are the main treatment options for scoliosis?
Treatment options for scoliosis can range from nonsurgical methods, such as observation with repeat X-rays, to surgical methods, such as spinal fusion.
What are the main treatment options for scoliosis?
This answer is adapted from the Gillette Children’s Healthcare Series book on Idiopathic Scoliosis.
Treatment options for scoliosis can range from nonsurgical methods, such as observation with repeat X-rays, to surgical methods, such as spinal fusion. Treatment options include the following:
- Observation: Regular spine X-rays and clinical exams with a spine specialist to monitor scoliosis curve for possible progression.
- Bracing: A spinal brace that applies corrective forces to the spine to slow or stop scoliosis curve progression.
- Casting: A full-torso cast (hardened plaster or fiberglass that must be cut off to remove) that applies corrective forces to the spine to improve the scoliosis curve (decrease the Cobb angle) or slow or stop scoliosis curve progression.
- Surgery: Surgery performed to prevent future progression and improve the scoliosis curve (decrease the Cobb angle). There are many types of scoliosis surgery. The most common type is spinal fusion, defined as fusing (joining together) two or more vertebrae in the spine; screws and metal rods are typically used to hold the spine in the straightened position and facilitate fusion between bones.
As the child grows, the risk of scoliosis progression may increase or decrease, resulting in treatment plans changing. It is common for an individual to undergo multiple treatment types over the course of their childhood and adolescence. For example, an individual may be observed for a period of time, then prescribed bracing treatment if their curve progresses.
The appropriate treatment chosen and the related goals depend primarily on individual patient goals and specific treatment indications. Indications include, but are not limited to, size of the curve, risk of curve progression, and skeletal maturity of the child.
Treatment indications and goals may vary at other hospitals and treatment centers. Surgical guidelines are general and depend on the surgery type and clinical practice continually evolves.
It is important to note that for most individuals, scoliosis cannot be “cured” (i.e., to achieve a Cobb angle less than 10 degrees). For some children with infantile idiopathic scoliosis, their curve may spontaneously resolve, or casting treatment can reduce the curve to less than 10 degrees, but that is the exception. The more common outcome and realistic goal is to have a small enough residual curve after treatment that will not adversely affect quality of life.
How effective is bracing at stopping curve progression in individual with idiopathic scoliosis?
In individuals with idiopathic scoliosis, two outcomes commonly used to measure bracing success are:
- Five degrees or less of curve progression during brace treatment
- Avoiding surgery (typically meaning that the Cobb angle does not progress to 50 degrees or more)
How effective is bracing at stopping curve progression in individual with idiopathic scoliosis?
This answer is adapted from the Gillette Children’s Healthcare Series book on Idiopathic Scoliosis.
In individuals with idiopathic scoliosis, two outcomes commonly used to measure bracing success are:
- Five degrees or less of curve progression during brace treatment
- Avoiding surgery (typically meaning that the Cobb angle does not progress to 50 degrees or more)
When a scoliosis curve progresses 6 degrees or more during brace treatment, or if surgery is recommended due to curve progression beyond 50 degrees, this may be called “treatment failure.” Successful bracing treatment in AIS is correlated with wear time. In a landmark multicenter, randomized controlled trial, two groups of individuals with AIS were studied: a full-time brace treatment group and an observation group that did not wear a brace. The brace treatment group was successful in preventing progression to 50 degrees 75 percent of the time compared to the observation group, which was successful only 42 percent of the time. Adolescents who wore the brace for more hours had a greater chance of success with brace treatment.
Although wear time is extremely important, the risk of treatment failure is not equal for all individuals with AIS, even with perfect adherence to the prescribed wear time. The following full-time brace failure risk factors have been identified for individuals with AIS:
- Poor adherence to prescribed full-time wear (less than 10 to 13 hours per day).
- Significant amount of growth remaining at the start of brace treatment (Risser 0, triradiate cartilage open). For example, individuals with open triradiate cartilage at baseline have a 30 percent greater risk of treatment failure than those with closed triradiate cartilage at baseline.
- Cobb angle greater than or equal to 40 degrees prior to reaching adolescent growth spurt. For example, individuals with a 40-degree curve at baseline had a 40 percent greater risk of treatment failure than individuals with a 25-degree curve at baseline.
- Poor correction of the scoliosis curve in the brace as seen on the first in-brace X-ray.
- Large amount of vertebral rotation (rotation of the spine in the axial plane).
- Curves in the thoracic region
- Osteopenia (a lower bone density than is typical for the individual’s age in the general population).
- Higher body mass index (BMI), which can make it difficult to achieve adequate brace fit and in-brace curve correction.
Knowing these risk factors, spine specialists choose appropriate candidates for brace treatment, meaning those who are most likely to benefit from wearing the brace. Clinical tools, such as risk calculators, can guide spine specialists, orthotists, individuals and their families in being able to assess the risk of progression by using their baseline characteristics. Together, they can decide if treatment with a brace is likely to be beneficial and therefore warranted.
How do we know if scoliosis surgery is necessary?
Surgery is generally only considered necessary for infantile idiopathic scoliosis when scoliosis curves progress to a severe degree that threatens spinal function, cardiopulmonary health, or quality of life.
How do we know if scoliosis surgery is necessary?
Surgery is generally only considered necessary for infantile idiopathic scoliosis when scoliosis curves progress to a severe degree that threatens spinal function, cardiopulmonary health, or quality of life. Depending on the individual, surgery may be recommended to decrease curve progression, improve the scoliosis curve (decrease the Cobb angle) while allowing continued spine and chest wall growth.
For Juvenile idiopathic scoliosis and adolescent idiopathic scoliosis surgical treatment may be considered necessary if the Cobb angle reaches or exceeds 45–50 degrees, especially if the curve continues to progress and is having a negative impact on the child’s health and quality of life.
This answer is adapted from the Gillette Children’s Healthcare Series book on Idiopathic Scoliosis.
Surgery is also typically considered when non-surgical treatments fail to stabilize the curve or when there is a high risk of further deterioration that would impact long-term health and function. The decision is made by a spine specialist using clinical evaluation, imaging (such as X-rays), and patient-specific factors like age, skeletal maturity, and curve pattern.
How do we know if surgery is necessary and what is recovery like?
Surgery is usually considered when the curve is large, progressive, and unlikely to be controlled with bracing or other non‑operative measures.
Spine specialists recommend a surgery only if they believe the benefits outweigh the potential risks for the individual. There are some thresholds that typically trigger a recommendation for operative treatment, especially in congenital scoliosis.
How do we know if surgery is necessary and what is recovery like?
This answer is adapted from the Gillette Children’s Healthcare Series book on Scoliosis. For more information see Scoliosis – Congenital Neuromuscular, Syndromic, and Other Nonidiopathic Types.
Surgery is usually considered when the curve is large, progressive, and unlikely to be controlled with bracing or other non‑operative measures.
Spine specialists recommend a surgery only if they believe the benefits outweigh the potential risks for the individual. There are some thresholds that typically trigger a recommendation for operative treatment, especially in congenital scoliosis:
- Age
- Curve magnitude – a Cobb angle > 40° is a common cut‑off for surgery.
- Progression pattern – a long, continuously worsening curve, or a structural abnormality that is known to keep growing (e.g., a fully segmented hemivertebra or a unilateral unsegmented bar)
These may lead the surgeon to operate prophylactically even before the curve reaches 40–50°, because the risk of future rapid progression is high. These criteria help clinicians decide whether the benefits of surgery outweigh the risks . There are risks with any surgery: surgical risks are things that may go wrong during or shortly after surgery while the individual is still in the hospital (in-hospital complications). Long-term complications are problems that may occur after the individual has been discharged from the hospital and may develop over the course of months or even years following surgery.
When other conditions are present in addition to scoliosis, it is difficult to give a “one size fits all” account of recovery after surgery. Following are some general pointers; the spine team will discuss specifics in relation to the individual’s surgery.
Common milestones that a patient must reach before they can leave the hospital after any type of scoliosis surgery include being able to tolerate being out of bed and mobilize well (safely move at the level they were prior to surgery), tolerate food, urinate and have a bowel movement, and achieve reasonable pain control with pain medications that can be taken at home. A standard three-day recovery schedule after scoliosis surgery may look like the following:
- Day of surgery: The patient may experience drowsiness and/or dizziness when waking up from general anesthesia. They will be able to eat ice chips while their stomach wakes up, and they eventually can begin to take small sips of clear liquid (assuming they were able to do this before surgery). Pain control will be a focus after surgery, with pain medicine administered through an IV connected to a medicine pump. Patients should be out of bed (e.g., standing or using their wheelchair) the evening of surgery with the assistance of care team members. This may be associated with light-headedness, nausea, or even vomiting, which is normal and will improve as a patient is up more often.
- Day one after surgery: The patient will continue being up and out of bed and mobilizing. IV pain medication will be switched to pain medication by mouth or G-tube. The urinary catheter will be The patient will slowly start advancing their diet to how they were feeding before surgery.
- Days two and three after surgery: The patient will continue to move and increase time out of bed so that they and their caregivers feel prepared for home. A physical therapist may educate caregivers on any modifications in transferring the patient after surgery. If the patient has a custom wheelchair, their seating system will be adjusted to accommodate their new spine posture and shape. Postoperative X-rays will be taken. The patient and family will receive any discharge medications and education materials about going home after surgery. Discharge paperwork will be signed, and then the patient can leave the hospital.
Patients and families are often concerned about pain after surgery. Pain is expected and is a normal part of healing. Pain is different for everyone, but patients often say the first three days after surgery are particularly challenging. Certain movements may be especially painful, and patients may require assistance with those movements for a week or so. The individual may also have muscle spasms throughout their body that feel like squeezing pain and tightness. This can be improved by changing position, getting up and moving around, using heating pads, and/or taking medications.
At discharge, families may be sent home with narcotics (opioids) and muscle relaxants. It is expected that the individual will be slowly weaned off these medications and that they will be discontinued 7 to 10 days after surgery. While narcotics are beneficial during this first week after surgery, they are strong medications that carry risks of dependence and addiction. As such, spine specialists advise discontinuing these as soon as this can be safely accomplished. The use of over-the-counter pain medications such as acetaminophen (called paracetamol in some countries) may be continued for another two to three weeks as needed.
Purchase ‘Scoliosis: Congenital, Neuromuscular, Syndromic and other Nonidiopathic Types’.
Preview full content of the book via Flipbook.
Submit a question
Let us know what other questions you have. Are there specific topics you would you like us to cover?
Contact us now using the form.
Plain Language Summaries
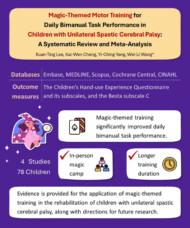
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to individuals with disabilities, parents, caregivers, and others. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
Helpful videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Contact us
Please feel free to contact us if you have any feedback or suggestions: