Welcome
Start exploring here! We hope this will be a useful resource to help you find the information you need about cerebral palsy and other childhood-onset disabilities. We want to help you to find answers to your questions – so please let us know what else you would like us to cover. Here we are presenting videos, summaries, research information and other resources.
Read on for more
Ways we can help
1
Family-friendly Books
Discover our collection of family-friendly books featuring accessible, research-based insights. These titles include the perspectives of families and individuals with lived experience, offering valuable guidance while supporting parents on their journey.
2
Free Chapters
We have selected a range of chapters from our books, offering helpful insights and practical tips. Our chapters summaries highlight key points. View the full chapter to explore each topic in more depth.
3
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
4
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to more people. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
5
Helpful Videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Gillette Children’s Healthcare Series
The goal of the Gillette Children’s Healthcare Series is to empower families through a greater understanding of their condition and therefore help optimize outcomes for children, adolescents and adults living with these childhood-acquired and largely lifelong conditions.

Free chapter downloads
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
How is cerebral palsy diagnosed, and what tests or assessments should I expect for my child?
There is no single test to confirm CP, unlike other conditions such as type 1 diabetes, which is confirmed through a simple blood test for glucose, or Down syndrome, which is confirmed through a genetic test.
How is cerebral palsy diagnosed, and what tests or assessments should I expect for my child?
This answer is adapted from the Gillette Children’s Healthcare Series books on Cerebral Palsy (CP).
There is no single test to confirm CP, unlike other conditions such as type 1 diabetes, which is confirmed through a simple blood test for glucose, or Down syndrome, which is confirmed through a genetic test. CP is not a single condition; rather, it is a group of conditions.
Until recently, a diagnosis of CP was generally made between 12 and 24 months based on a combination of clinical signs (e.g., lack of use of a limb), neurological symptoms (e.g., presence of spasticity), and physical limitations (e.g., delayed independent sitting or walking). However, using certain standardized tests in combination with clinical examination and medical history a diagnosis of CP can often accurately be made before six months corrected age. Early diagnosis is very important because it allows for early intervention, which helps to achieve better functional outcomes for the child.
There are two distinct pathways in the International Clinical Practice Guideline for early diagnosis of CP:
Before five months corrected age, for infants with newborn detectable risk factors (e.g., preterm):
- MRI (magnetic resonance imaging)
- GMs (Prechtl Qualitative Assessment of General Movements)
- HINE (Hammersmith Infant Neurological Examination)
After five months corrected age for infants with infant detectable risk factors (e.g., delayed motor milestones)
- MRI
- HINE
- DAYC (Developmental Assessment of Young Children)
The presence of a brain injury is confirmed by MRI in many but not all children with CP. Imaging may also help determine when the brain injury occurred. However, up to 17 percent of children diagnosed with CP have normal MRI brain scans. For these children, best practice is to investigate further to rule out genetic and metabolic conditions.
Where a CP diagnosis is suspected but cannot be made with certainty, using the interim diagnosis of “high risk for CP” is recommended until a diagnosis is confirmed. This allows the child to receive the benefits of CP-specific early intervention.
For further information, pleas check the Mac Keith Press title Prechtl’s Method on the Qualitative Assessment of General Movements in Preterm, Term and Young Infants and the Hammersmith Neonatal and Infant Neurological Examinations.
- Purchase 'Spastic Hemiplegia–Unilateral Cerebral Palsy'
- Preview full content of 'Spastic Hemiplegia–Unilateral Cerebral Palsy' via Flipbook.
- Purchase 'Spastic Diplegia–Bilateral Cerebral Palsy 2nd Edition'
- Preview full content of 'Spastic Diplegia–Bilateral Cerebral Palsy 2nd Edition' via Flipbook.
- Purchase 'Spastic Quadriplegia–Bilateral Cerebral Palsy'
- Preview full content of 'Spastic Quadriplegia–Bilateral Cerebral Palsy' via Flipbook.
How early can cerebral palsy be diagnosed?
Cerebral palsy (CP) can often be diagnosed before six months corrected age. Research indicates that a diagnosis can be made with reasonable accuracy using Magnetic resonance imaging (MRI) in combination with standardized assessments like the Prechtl Qualitative Assessment of General Movements (GMs) and the Hammersmith Infant Neurological Examination (HINE).
How early can cerebral palsy be diagnosed?
This answer is adapted from the Gillette Children’s Healthcare Series books on Cerebral Palsy (CP).
Cerebral palsy (CP) can often be diagnosed before six months corrected age. Research indicates that a diagnosis can be made with reasonable accuracy using Magnetic resonance imaging (MRI) in combination with standardized assessments like the Prechtl Qualitative Assessment of General Movements (GMs) and the Hammersmith Infant Neurological Examination (HINE). These tools are used for infants with known risk factors, such as preterm birth or birth asphyxia. Early diagnosis is very important because it allows for early intervention, which helps to achieve better functional outcomes for the child.
For further information, pleas check the Mac Keith Press title Prechtl’s Method on the Qualitative Assessment of General Movements in Preterm, Term and Young Infants and the Hammersmith Neonatal and Infant Neurological Examinations.
- Purchase 'Spastic Hemiplegia–Unilateral Cerebral Palsy'
- Preview full content of 'Spastic Hemiplegia–Unilateral Cerebral Palsy' via Flipbook.
- Purchase 'Spastic Diplegia–Bilateral Cerebral Palsy 2nd Edition'
- Preview full content of 'Spastic Diplegia–Bilateral Cerebral Palsy 2nd Edition' via Flipbook.
- Purchase 'Spastic Quadriplegia–Bilateral Cerebral Palsy'
- Preview full content of 'Spastic Quadriplegia–Bilateral Cerebral Palsy' via Flipbook.
What is early intervention in cerebral palsy?
Early intervention refers to a range of therapies and support services provided to children with CP (or at high risk of CP) from birth to age two and sometimes beyond.
What is early intervention in cerebral palsy?
This answer is adapted from the Gillette Children’s Healthcare Series books on Cerebral Palsy (CP).
Early intervention refers to a range of therapies and support services provided to children with CP (or at high risk of CP) from birth to age two and sometimes beyond.
CP-specific early interventions are designed to:
- Optimize motor, cognition, and communication skills using interventions that promote learning and neuroplasticity
- Prevent secondary impairments and minimize complications that worsen function or interfere with learning (e.g., monitor hips, control epilepsy, take care of sleeping, feeding)
- Promote parent or caregiver coping and mental health
Neuroplasticity (also known as brain plasticity, neural plasticity, and neuronal plasticity) refers to the brain’s ability to change. After a brain injury occurs, the brain will try to recover somewhat by creating new pathways around the injury, moving functions to a healthy area of the brain, or strengthening existing healthy connections. This potential for change and growth through practice and repetition allows the brain to develop new skills.
Neuroplasticity is at its optimum during early brain development. The first thousand days are a critical time for brain development; this is a time when interventions are particularly effective. This is also a time of extreme vulnerability: the same neuroplasticity that gives a child the potential to recover function also makes them very sensitive to any intervention, which can result in unwanted consequences unless the intervention has been proven safe.
- Purchase 'Spastic Hemiplegia–Unilateral Cerebral Palsy'
- Preview full content of 'Spastic Hemiplegia–Unilateral Cerebral Palsy' via Flipbook.
- Purchase 'Spastic Diplegia–Bilateral Cerebral Palsy 2nd Edition'
- Preview full content of 'Spastic Diplegia–Bilateral Cerebral Palsy 2nd Edition' via Flipbook.
- Purchase 'Spastic Quadriplegia–Bilateral Cerebral Palsy'
- Preview full content of 'Spastic Quadriplegia–Bilateral Cerebral Palsy' via Flipbook.
How does cerebral palsy affect my child?
Cerebral palsy (CP) is a group of conditions caused by an injury to the developing brain, which can result in a variety of motor and other problems that affect how the child functions. Because the injury occurs in a developing brain and growing child, problems often change over time, even though the brain injury itself is unchanging.
How does cerebral palsy affect my child?
This answer is adapted from the Gillette Children’s Healthcare Series books on Cerebral Palsy (CP).
CP is a group of conditions caused by an injury to the developing brain, which can result in a variety of motor and other problems that affect how the child functions. Because the injury occurs in a developing brain and growing child, problems often change over time, even though the brain injury itself is unchanging.
Motor problems affect the ability to move and the quality of those movements.
A proportion of children with CP have problems in the areas of speech, intelligence, (cognition), vision, epilepsy, and hearing. The prevalence and severity of these problems were found to be greater in children at higher GMFCS levels compared with those at lower GMFCS levels.
- Purchase 'Spastic Hemiplegia–Unilateral Cerebral Palsy'
- Preview full content of 'Spastic Hemiplegia–Unilateral Cerebral Palsy' via Flipbook.
- Purchase 'Spastic Diplegia–Bilateral Cerebral Palsy 2nd Edition'
- Preview full content of 'Spastic Diplegia–Bilateral Cerebral Palsy 2nd Edition' via Flipbook.
- Purchase 'Spastic Quadriplegia–Bilateral Cerebral Palsy'
- Preview full content of 'Spastic Quadriplegia–Bilateral Cerebral Palsy' via Flipbook.
Submit a question
Let us know what other questions you have. Are there specific topics you would you like us to cover?
Contact us now using the form.
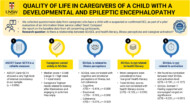
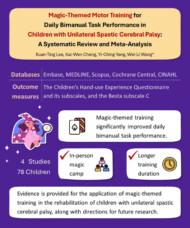
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to individuals with disabilities, parents, caregivers, and others. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
Helpful videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Contact us
Please feel free to contact us if you have any feedback or suggestions: