Welcome
Start exploring here! We hope this will be a useful resource to help you find the information you need about cerebral palsy and other childhood-onset disabilities. We want to help you to find answers to your questions – so please let us know what else you would like us to cover. Here we are presenting videos, summaries, research information and other resources.
Read on for more
Ways we can help
1
Family-friendly Books
Discover our collection of family-friendly books featuring accessible, research-based insights. These titles include the perspectives of families and individuals with lived experience, offering valuable guidance while supporting parents on their journey.
2
Free Chapters
We have selected a range of chapters from our books, offering helpful insights and practical tips. Our chapters summaries highlight key points. View the full chapter to explore each topic in more depth.
3
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
4
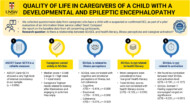
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to more people. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
5
Helpful Videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Gillette Children’s Healthcare Series
The goal of the Gillette Children’s Healthcare Series is to empower families through a greater understanding of their condition and therefore help optimize outcomes for children, adolescents and adults living with these childhood-acquired and largely lifelong conditions.

Free chapter downloads
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
What does long-term outlook look like for children with craniosynostosis?
The long-term outlook for children with craniosynostosis is generally positive, particularly for those with nonsyndromic forms.
What does long-term outlook look like for children with craniosynostosis?
This answer is adapted from the Gillette Children’s Healthcare Series book on Craniosynostosis.
The long-term outlook for children with craniosynostosis is generally positive, particularly for those with nonsyndromic forms.
- Nonsyndromic Craniosynostosis: For children with nonsyndromic craniosynostosis who have undergone successful surgical repair, the long-term outlook is typically favorable. They can expect a typical life, with most requiring only a single surgery before their first birthday. Children with nonsyndromic CS (surgically repaired) age 7 to 16 years have a similar health-related quality of life (HRQOL) compared to typical children, and no major differences have been noted. Over 90 percent of children with nonsyndromic CS will not require any additional surgeries, and any remaining asymmetry is often not noticeable
- Syndromic Craniosynostosis: The long-term outlook for children with syndromic craniosynostosis is more complex and varies significantly depending on the specific syndrome. These children often require multiple surgeries throughout childhood and into adulthood to address the skull, face, and other associated medical issues. While they may face challenges related to cognition, behavior, speech, and other organ systems, they can still have a fulfilling life. The family and medical team work together to manage the condition, and children can participate in sports and activities as much as possible, with modifications when needed.
What is the difference between a seizure and epilepsy?
A seizure is an unexpected event caused by abnormal electrical activity in the brain, which may lead to sudden changes in movement, behavior, sensation, memory, or feelings. A single seizure, especially if provoked, does not mean a person has epilepsy.
What is the difference between a seizure and epilepsy?
This answer is adapted from chapter 1 of the Gillette Children’s Healthcare Series book on Epilepsy, understanding and managing the condition: a practical guide for families.
A seizure is an unexpected event caused by abnormal electrical activity in the brain, which may lead to sudden changes in movement, behavior, sensation, memory, or feelings. Experiencing or witnessing a seizure can be frightening, as it may involve jerking, shaking, twisting, or more subtle symptoms that are not always visible. Seizures can be provoked—triggered by factors such as fever, infection, electrolyte imbalance, or head injury—or unprovoked, occurring without an immediate cause. A single seizure, especially if provoked, does not mean a person has epilepsy.
Epilepsy, by contrast, is a medical condition defined by a tendency to have recurrent, unprovoked seizures. While epilepsy can occur at any age, it often begins in childhood or adolescence and understanding the difference between seizures (a single event) and epilepsy (a chronic condition) helps families feel more in control when navigating a diagnosis.
What are some other events that look like epileptic seizures but are not seizures?
Some events that look like seizures but are not seizures are referred to as “seizure mimics” or “nonepileptic events”. These events can resemble seizures clinically but are not caused by abnormal electrical activity in the brain . Differential diagnosis is used to distinguish between true seizures and these mimics.
What are some other events that look like epileptic seizures but are not seizures?
This answer is adapted from section 1.4 of the Gillette Children’s Healthcare Series book on Epilepsy, understanding and managing the condition: a practical guide for families.
Some events that look like seizures but are not seizures are referred to as “seizure mimics” or “nonepileptic events”. These events can resemble seizures clinically but are not caused by abnormal electrical activity in the brain . Differential diagnosis is used to distinguish between true seizures and these mimics.
The key differences in symptoms between actual seizures and seizure mimics lie in the nature of the event, associated features, and how they respond to certain behaviors or stimuli. For example:
- Seizures often involve uncontrolled, abnormal electrical activity in the brain, which may result in altered consciousness, involuntary movements (like jerking or shaking), sensory changes, or emotional experiences. These events typically have an abrupt onset and cannot be voluntarily controlled.
- Seizure mimics, on the other hand, may include conditions such as:
- Tics and stereotypes, which may be momentarily suppressed by the individual—unlike seizures, which are not under voluntary control.
- Psychological or psychiatric conditions, such as panic attacks, hyperventilation, dissociative disorders, or episodic dyscontrol, which may be triggered by stress and typically do not involve a true change in consciousness.
- Cardiovascular events, such as heart rhythm abnormalities (e.g., long QT syndrome) or postural orthostatic changes, which can cause fainting or loss of consciousness but are not due to brain electrical activity.
Additionally, features like duration, presence of triggers, level of consciousness, and response to external stimuli (e.g., ability to be interrupted) help differentiate seizures from mimics. A thorough evaluation of the event’s context—such as sounds, posture, movements, and emotional state—is essential for accurate diagnosis.
For more information see the book. You can preview the full content of the book via the Flipbook on the product page.
What should I do if my child has an epileptic seizure?
If your child has a seizure, follow the seizure first aid guidelines provided by the Epilepsy Foundation, using the code STAY, SAFE, SIDE.
What should I do if my child has an epileptic seizure?
This answer is adapted from the Gillette Children’s Healthcare Series book on Epilepsy, understanding and managing the condition: a practical guide for families.
If your child has a seizure, follow the seizure first aid guidelines provided by the Epilepsy Foundation, using the code STAY, SAFE, SIDE:
- Stay with your child and remain calm. Do not leave them alone during the seizure.
- Keep them safe by removing nearby objects that could cause injury. Do not restrain them and do not put any objects in their mouth.
- Place them on their side, keeping their airway clear. Remove any tight clothes around the neck and put something small and soft under their head.
After the seizure, stay with your child, monitor their breathing, and provide reassurance. Call emergency services if it’s their first seizure, if the seizure lasts longer than 5 minutes, or occurs in water. Always seek medical evaluation after a first-time seizure to determine the cause and appropriate treatment.
Learn more about seizure first aid at epilepsy.com/firstaid
Submit a question
Let us know what other questions you have. Are there specific topics you would you like us to cover?
Contact us now using the form.
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to individuals with disabilities, parents, caregivers, and others. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
Helpful videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Contact us
Please feel free to contact us if you have any feedback or suggestions: