Welcome
Start exploring here! We hope this will be a useful resource to help you find the information you need about cerebral palsy and other childhood-onset disabilities. We want to help you to find answers to your questions – so please let us know what else you would like us to cover. Here we are presenting videos, summaries, research information and other resources.
Read on for more
Ways we can help
1
Family-friendly Books
Discover our collection of family-friendly books featuring accessible, research-based insights. These titles include the perspectives of families and individuals with lived experience, offering valuable guidance while supporting parents on their journey.
2
Free Chapters
We have selected a range of chapters from our books, offering helpful insights and practical tips. Our chapters summaries highlight key points. View the full chapter to explore each topic in more depth.
3
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
4
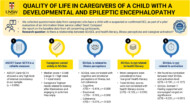
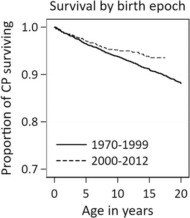
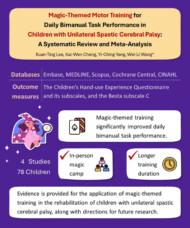
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to more people. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
5
Helpful Videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Gillette Children’s Healthcare Series
The goal of the Gillette Children’s Healthcare Series is to empower families through a greater understanding of their condition and therefore help optimize outcomes for children, adolescents and adults living with these childhood-acquired and largely lifelong conditions.

Free chapter downloads
The Knowledge Bank
Explore the answers to your questions here. Find out more about conditions, treatments, interventions, and all aspects of care. Follow signposts to find more in-depth, evidence-based information from Mac Keith Press content, as well as other great sources of knowledge.
What are the different types of epileptic seizures?
The different types of seizures are categorized based on where they begin in the brain and how they affect consciousness and movement.
What are the different types of epileptic seizures?
This answer is adapted from section 2.3 of the Gillette Children’s Healthcare Series book on Epilepsy, understanding and managing the condition: a practical guide for families.
A seizure is first classified based on where it begins in the brain, termed the “seizure onset zone”.
- Focal onset seizures (also called focal seizures) begin in one area of the brain.
- Generalized onset seizures involve both sides of the brain from the start.
- Unknown onset seizure: A seizure with an unclear starting location in the brain. The seizure is either focal onset or generalized onset, but the exact onset zone cannot be determined. Seizures classified as unknown may be later classified as focal onset or generalized onset if more testing identifies the onset zone.
Some seizures may start as focal and then spread to involve both sides of the brain
.The second classification is based on the level of awareness during a seizure. The level of awareness is the individual’s state of consciousness during a seizure and includes their “knowledge of self or environment.”
- Aware: The individual does not experience a loss of consciousness and is aware that a seizure is happening. They may even be able to carry on a conversation or complete a task during a seizure. They are also likely to recall the events during a seizure after it ends.
- Impaired awareness: The individual may appear confused, is not aware a seizure is occurring, may not be able to respond, or may experience a loss of consciousness. After the seizure ends, the individual will typically not be able to fully recall the event.
Focal onset seizures are either aware or impaired awareness seizures. However, all generalized onset seizures are presumed to have impaired awareness.
The third classification is based on the signs and symptoms of the seizure—what the seizure “looks” like, or how the individual feels or acts during the seizure. These are known as motor (movement) signs and nonmotor (without movement) signs and symptoms:
Motor signs are uncontrolled physical movements experienced by the individual during the seizure that can be seen by others observing the individual. Nonmotor signs and symptoms are what the individual who is seizing experiences. These may be observed by others if they include a lack of movement, emotional outbursts, or a change in vital signs.
What happens in the brain during an epileptic seizure?
During a seizure, there is uncontrolled, abnormal electrical activity in the brain that originates in networks of multiple neurons, not just a single neuron. This abnormal activity disrupts the brain’s normal ability to regulate signals, leading to sudden, excessive, and synchronous firing of neurons.
What happens in the brain during an epileptic seizure?
This answer is adapted from chapter 3 of the the Gillette Children’s Healthcare Series book on Epilepsy, understanding and managing the condition: a practical guide for families.
Neurons are the smallest unit of the nervous system, and there are billions of them in the brain and spinal cord. They are electrically excitable cells and carry information (signals) between the central nervous system and the rest of the body as electrical impulses through a web-like structure from neuron to neuron, or from neurons to other cells in the body.
During a seizure, there is uncontrolled, abnormal electrical activity in the brain that originates in networks of multiple neurons, not just a single neuron. This abnormal activity disrupts the brain’s normal ability to regulate signals, leading to sudden, excessive, and synchronous firing of neurons. The electrical activity may manifest as changes in movement, sensation, awareness, or behavior.
Seizures occur when the seizure threshold—the level of electrical activity required to trigger a seizure—is reached. Neurons communicate via synapses, and during a seizure, this communication becomes disrupted, with some neurons being overstimulated (excited) and others inhibited, leading to the chaotic brain activity seen during a seizure.
The abnormal electrical patterns can be detected using an EEG, which may show epileptiform discharges—distinct waveform patterns associated with epileptic activity. These discharges may occur during a seizure (ictal) or between seizures (interictal). The underlying cause of the abnormal activity may be related to genetic, structural, or metabolic factors, but the result is a breakdown in typical brain function during the event.
What happens during an EEG test?
During an EEG test, electrodes are placed on the scalp to measure and record the brain’s electrical activity, generating a visual graph of brain waves. The test is used to detect abnormal electrical patterns that may indicate epilepsy or other neurological conditions.
What happens during an EEG test?
This answer is adapted from chapter 4 of the Gillette Children’s Healthcare Series book on Epilepsy, understanding and managing the condition: a practical guide for families. Purchase the book here.
During an EEG test, electrodes are placed on the scalp to measure and record the brain’s electrical activity, generating a visual graph of brain waves. The test is used to detect abnormal electrical patterns that may indicate epilepsy or other neurological conditions.
The EEG may be performed with simultaneous video recording (called video EEG or VEEG), which allows healthcare providers to observe the individual’s behavior and movements while recording brain activity. This helps distinguish between seizures and events that resemble seizures but are not caused by abnormal electrical discharges.
The medical professional evaluates the brain wave patterns, as well as the individual’s level of awareness, motor signs, and nonmotor symptoms during the recording.
EEG records only live events, however, so it is possible that no events will occur during the EEG. If certain triggers are identified for the individual, those can be used to try to induce a seizure during EEG. Watching flashing lights, hyperventilating (breathing rapidly), closing eyes, opening eyes, and other actions are often performed during EEG to try and trigger an event. Medical professionals may also request that the individual be sleep deprived since lack of sleep may be a trigger for seizures. Some seizures occur more often with sleep, so an overnight stay in the hospital may help capture events related to sleep. EEG can be done in either outpatient or inpatient settings. Typically, an outpatient EEG test lasts from 20 minutes to several hours, and an inpatient
EEG test lasts from one to several days (or weeks in rare instances).
What are the causes of epilepsy?
The causes of epilepsy include structural, genetic, infectious, metabolic, and immune factors. Or, as in approximately 50 percent of epilepsy cases worldwide the cause can remain unknown. Determining the cause, when possible, helps guide management and can provide clues to long-term prognosis.
What are the causes of epilepsy?
This answer is adapted from chapter 6 of the Gillette Children’s Healthcare Series book on Epilepsy, understanding and managing the condition: a practical guide for families. Purchase the book here.
The causes of epilepsy include structural, genetic, infectious, metabolic, and immune factors. Or, as in approximately 50 percent of epilepsy cases worldwide the cause can remain unknown. Determining the cause, when possible, helps guide management and can provide clues to long-term prognosis.
Structural epilepsy results from a distinct brain abnormality, such as a lesion or tumor, and often presents with focal onset seizures.
Genetic epilepsy is caused by or closely associated with changes in genes, which may be inherited or occur as new mutations (de novo). It is often suspected when epilepsy begins very early in life and can present with any seizure type.
Infectious causes may include conditions like meningitis or encephalitis, while metabolic causes can involve imbalances in blood sugar, electrolytes, or other body chemicals.
Immune-related causes involve autoimmune processes that affect the brain and may trigger seizures.
Submit a question
Let us know what other questions you have. Are there specific topics you would you like us to cover?
Contact us now using the form.
Plain Language Summaries
Plain language summaries are an effective way of communicating scientific research to a wider audience. By presenting the key findings and significance of a study in easy-to-understand language, the content becomes more accessible to individuals with disabilities, parents, caregivers, and others. Here we present summaries of papers published in Developmental Medicine & Child Neurology (DMCN).
Helpful videos
Here you will find a collection of short videos from authors and editors summarising their work. They cover Developmental Medicine & Child Neurology (DMCN) articles, Mac Keith Press books and e-learning. The aim of the videos is to help viewers get a clear understanding of why the research is important, how it was carried out, and real-world implications.
Contact us
Please feel free to contact us if you have any feedback or suggestions: